W.H.O. Still In Process Of Secret IHR Amendment Negotiations To Eliminate "Respect For Dignity & Human Rights"! Part 5: Reminding W.H.O. Of Their Duties Under Human Rights Law!
On May 2, 2022 IOJ presented the old WHO to the new WHO with some suggestions for reform, and a demand to dispute us & Dr. Yeadon! Formal charges are heating up. With public support we can win this.
We know this post is very long (albeit extremely important) and for those who do not have time to read the entire post, the summary is:
W.H.O. originally agreed to fundamental obligations which entail protection of respect for dignity, human rights and final freedoms
W.H.O. recognizes our International Organization Interest Of Justice as a stakeholder in “Pandemic Preparedness and Response” and we are fighting for the right to meaningfully participate in the design and drafting of the W.H.O. pandemic treaty and also to protest the IHR amendments which seek to undermine humanity’s dignity and human rights by oppression and enslavement by removing fundamental freedoms.
In May of 2022, Interest Of Justice began a formal legal protest against the actions of the W.H.O., including their merger with World Economic Forum (WEF) due to the appearance of conflicts of interest, imbalance of power, and obvious monopolistic tendencies, which should be prohibited in the public interest.
On November 30, 2022 interest of justice filed formal charges against the world health organization, Director general and chief scientist as well as her successor. As of today, the world health organization and their allegedly independent oversight, promised to respond within seven days and went into hiding, never responding, therefore, we presume all presumptions in the in the stakeholder engagement package provided below stand as true.
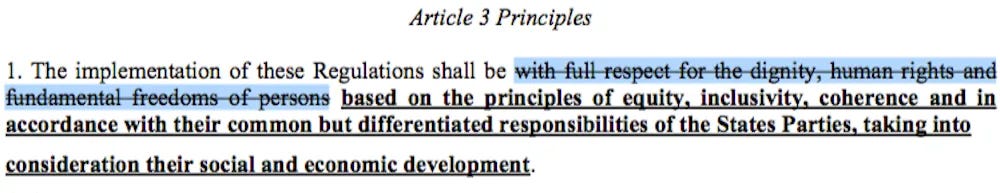
The final formal charges are being drafted right now to combat the IHR amendments which would outrageously remove dignity, human rights and federal freedoms from public health policy. The charges include many issues, including we have alleged with no dispute that fraudulent PCR statistics have been intentionally fabricated using the first W.H.O. diagnostics guidance created by Christian Drosten at Charite Germany, to declare an emergency in bad faith which violates international law. We are alleging that this is an internationally, wrongful act, which obligates the world health organization to the duty of cessation, compensation, satisfaction (apology) and the assurance of non-repetition.
These charges and the next upcoming legal steps we are about to take are a big deal to YOUR freedoms and dignity now and into the future.
Read below to see the detailed document on the desk of Director General of the W.H.O. and chief scientist as well as the independent oversight in charge of the investigation for breach of duty and crimes against humanity.
Read the legal stakeholder document below to learn about what W.H.O. has promised in regards to your human rights!
Learn about our rights as W.H.O. recognized stakeholders to DEFEND your dignity, human rights and fundamental freedoms!
PART 5: ON MAY 2, 2022 WE SENT A HUGE LEGAL PACKET TO THE WHO
This is a long explanatory post. Skip below to read it.
We posted in 6 parts to explain what we sent the WHO on May 2, 2022 and exactly what is currently legally in process as of today between IOJ team and the W.H.O.:
1. Open Letter, which is what we sent the W.H.O. on May 2, 2022. Read Here >
2. Stakeholder engagement packet - Memorandum of Understanding of stakeholder engagement (very interesting to know our POWER) Read Here>
3. Rebuttal to Tedros opening remark Public Hearings Read Here>
4. Rebuttal to Tedros closing statement Public Hearings Read Here >
5. Memorandum of Understanding regarding Human rights and health Duties of the WHO. YOU ARE HERE >
6. Costa Rica’s unresponsive health system under the W.H.O.. Read Here > (COMING Next)
BELOW IS PART OF THE PACKET WE SENT THE W.H.O. ON MAY 2, 2022 (in legal proceedings now against W.H.O.).
VERBATIM:
Memorandum of Understanding regarding Human rights and health Duties of the W.H.O.
Key facts
The W.H.O. Constitution (1946) envisages “…the highest attainable standard of health as a fundamental right of every human being.”
Understanding health as a human right creates a legal obligation on states to ensure access to timely, acceptable, and affordable health care of appropriate quality as well as to providing for the underlying determinants of health, such as safe and potable water, sanitation, food, housing, health-related information and education, and gender equality.
A States’ obligation to support the right to health – including through the allocation of “maximum available resources” to progressively realize this goal - is reviewed through various international human rights mechanisms, such as the Universal Periodic Review, or the Committee on Economic, Social and Cultural Rights. In many cases, the right to health has been adopted into domestic law or Constitutional law.
A rights-based approach to health requires that health policy and programs must prioritize the needs of those furthest behind first towards greater equity, a principle that has been echoed in the recently adopted 2030 Agenda for Sustainable Development and Universal Health Coverage. (1)
The right to health must be enjoyed without discrimination on the grounds of race, age, ethnicity or any other status. Non-discrimination and equality requires states to take steps to redress any discriminatory law, practice or policy.
Another feature of rights-based approaches is meaningful participation. Participation means ensuring that national stakeholders – including non-state actors such as non-governmental organizations – are meaningfully involved in all phases of programming: assessment, analysis, planning, implementation, monitoring and evaluation.
“The right to the highest attainable standard of health” implies a clear set of legal obligations on states to ensure appropriate conditions for the enjoyment of health for all people without discrimination.
The right to health is one of a set of internationally agreed human rights standards, and is inseparable or ‘indivisible’ from these other rights. This means achieving the right to health is both central to, and dependent upon, the realization of other human rights, to food, housing, work, education, information, and participation.
The right to health, as with other rights, includes both freedoms and entitlements:
Freedoms include the right to control one’s health and body (for example, sexual and reproductive rights) and to be free from interference (for example, free from torture and non-consensual medical treatment and experimentation).
Entitlements include the right to a system of health protection that gives everyone an equal opportunity to enjoy the highest attainable level of health.
Focus on disadvantaged populations
Disadvantage and marginalization serve to exclude certain populations in societies from enjoying good health. Three of the world’s most fatal communicable diseases – malaria, HIV/AIDS and tuberculosis – disproportionately affect the world’s poorest populations, and in many cases are compounded and exacerbated by other inequalities and inequities including gender, age, sexual orientation or gender identity and migration status. Conversely the burden of non-communicable diseases – often perceived as affecting high-income countries – is increasing disproportionately among lower-income countries and populations, and is largely associated with lifestyle and behaviour factors as well as environmental determinants, such as safe housing, water and sanitation that are inextricably linked to human rights.
A focus on disadvantage also reveals evidence of those who are exposed to greater rates of ill-health and face significant obstacles to accessing quality and affordable healthcare, including indigenous populations. While data collection systems are often ill-equipped to capture data on these groups, reports show that these populations have higher mortality and morbidity rates, due to noncommunicable diseases such as cancer, cardiovascular diseases, and chronic respiratory disease. These populations may also be the subject of laws and policies that further compound their marginalization and make it harder for them to access healthcare prevention, treatment, rehabilitation and care services.
Violations of human rights in health
Violations or lack of attention to human rights can have serious health consequences. Overt or implicit discrimination in the delivery of health services – both within the health workforce and between health workers and service users – acts as a powerful barrier to health services, and contributes to poor quality care.
Mental ill-health often leads to a denial of dignity and autonomy, including forced treatment or institutionalization, and disregard of individual legal capacity to make decisions. Paradoxically, mental health is still given inadequate attention in public health, in spite of the high levels of violence, poverty and social exclusion that contribute to worse mental and physical health outcomes for people with mental health disorders.
Violations of human rights not only contribute to and exacerbate poor health, but for many, including people with disabilities, indigenous populations, women living with HIV, sex workers, people who use drugs, transgender and intersex people, the health care setting presents a risk of heightened exposure to human rights abuses – including coercive or forced treatment and procedures.
Human rights-based approaches
A human rights-based approach to health provides a set of clear principles for setting and evaluating health policy and service delivery, targeting discriminatory practices and unjust power relations that are at the heart of inequitable health outcomes.
In pursuing a rights-based approach, health policy, strategies and programmes should be designed explicitly to improve the enjoyment of all people to the right to health, with a focus on the furthest behind first. The core principles and standards of a rights-based approach are detailed below.
Core principles of human rights
Accountability
States and other duty-bearers are answerable for the observance of human rights. However, there is also a growing movement recognising the importance of other non-state actors such as businesses in the respect and protection of human rights. (2)
Equality and non-discrimination
The principle of non-discrimination seeks ‘…to guarantee that human rights are exercised without discrimination of any kind based on race, colour, sex, language, religion, political, or other opinion, national or social origin, property, birth or other status such as disability, age, marital and family status, sexual orientation and gender identity, health status, place of residence, economic and social situation’.
Any discrimination, for example in access to health care, as well as in means and entitlements for achieving this access, is prohibited on the basis of race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth, physical or mental disability, health status (including HIV/AIDS), sexual orientation ,and civil, political, social or other status, which has the intention or effect of impairing the equal enjoyment or exercise of the right to health.
The principle of non-discrimination and equality requires WHO to address discrimination in guidance, policies, and practices, such as relating to the distribution and provision of resources and health services. Non-discrimination and equality are key measures required to address the social determinants affecting the enjoyment of the right to health. Functioning national health information systems and availability of disaggregated data are essential to be able to identify the most vulnerable groups and diverse needs.
Participation
Participation requires ensuring that all concerned stakeholders including non-state actors have ownership and control over development processes in all phases of the programming cycle: assessment, analysis, planning, implementation, monitoring, and evaluation. Participation goes well beyond consultation or a technical addition to project design; it should include explicit strategies to empower citizens, especially the most marginalized, so that their expectations are recognised by the State.
Participation is important to accountability as it provides “…checks and balances which do not allow unitary leadership to exercise power in an arbitrary manner”.
Universal, indivisible and interdependent
Human rights are universal and inalienable. They apply equally, to all people, everywhere, without distinction. Human Rights standards – to food, health, education, to be free from torture, inhuman or degrading treatment – are also interrelated. The improvement of one right facilitates advancement of the others. Likewise, the deprivation of one right adversely affects the others.
Core elements of a right to health
Progressive realization using maximum available resources
No matter what level of resources they have at their disposal, progressive realisation requires that governments take immediate steps within their means towards the fulfilment of these rights. Regardless of resource capacity, the elimination of discrimination and improvements in the legal and juridical systems must be acted upon with immediate effect.
Non-retrogression
States should not allow the existing protection of economic, social, and cultural rights to deteriorate unless there are strong justifications for a retrogressive measure. For example, introducing school fees in secondary education which had formerly been free of charge would constitute a deliberate retrogressive measure. To justify it, a State would have to demonstrate that it adopted the measure only after carefully considering all the options, assessing the impact and fully using its maximum available resources.
Core components of the right to health
The right to health (Article 12) was defined in General Comment 14 of the Committee on Economic, Social and Cultural Rights – a committee of Independent Experts, responsible for overseeing adherence to the Covenant. (4) The right includes the following core components:
Availability
Refers to the need for a sufficient quantity of functioning public health and health care facilities, goods and services, as well as programmes for all. Availability can be measured through the analysis of disaggregated data to different and multiple stratifiers including by age, sex, location and socio-economic status and qualitative surveys to understand coverage gaps and health workforce coverage
Accessibility
Requires that health facilities, goods, and services must be accessible to everyone. Accessibility has four overlapping dimensions:
non-discrimination
physical accessibility
economical accessibility (affordability)
information accessibility.
Assessing accessibility may require analysis of barriers – physical financial or otherwise – that exist, and how they may affect the most vulnerable, and call for the establishment or application of clear norms and standards in both law and policy to address these barriers, as well as robust monitoring systems of health-related information and whether this information is reaching all populations.
Acceptability
Relates to respect for medical ethics, culturally appropriate, and sensitivity to gender. Acceptability requires that health facilities, goods, services and programmes are people-centred and cater for the specific needs of diverse population groups and in accordance with international standards of medical ethics for confidentiality and informed consent.
Quality
Facilities, goods, and services must be scientifically and medically approved. Quality is a key component of Universal Health Coverage, and includes the experience as well as the perception of health care. Quality health services should be:
Safe – avoiding injuries to people for whom the care is intended;
Effective – providing evidence-based healthcare services to those who need them;
People-centred – providing care that responds to individual preferences, needs and values;
Timely – reducing waiting times and sometimes harmful delays.
Equitable – providing care that does not vary in quality on account of gender, ethnicity, geographic location, and socio-economic status;
Integrated – providing care that makes available the full range of health services throughout the life course;
Efficient – maximizing the benefit of available resources and avoiding waste
WHO response TO HUMAN RIGHTS
WHO has claimed to make a commitment to mainstream human rights into healthcare programmes and policies on national and regional levels by looking at underlying determinants of health as part of a comprehensive approach to health and human rights.
In addition, WHO has allegedly been actively strengthening its role in providing technical, intellectual, and political leadership on the right to health including:
strengthening the capacity of WHO and its Member States to integrate a human rights-based approach to health;
advancing the right to health in international law and international development processes; and
advocating for health-related human rights, including the right to health.
Addressing the needs and rights of individuals at different stages across the life course requires taking a comprehensive approach within the broader context of promoting human rights, gender equality, and equity.
As such, WHO promotes a concise and unifying framework that builds on existing approaches in gender, equity, and human rights to generate more accurate and robust solutions to health inequities. The integrated nature of the framework is an opportunity to build on foundational strengths and complementarities between these approaches to create a cohesive and efficient approach to promote health and well-being for all.
Executive summary
The way public health systems finance and interact with multinational public-private monopolies and individuals can impact on the well-being of both the individual and society. WHO has termed this work health system "responsiveness" and has proposed that a health system's performance in this area also be evaluated alongside the measurement of health system performance with more traditional indicators like mortality, morbidity and utilization statistics.
If a health system is responsive, it is possible that interactions people have within the health system will improve their well-being, irrespective of improvements to their health.
The concept of responsiveness has been operationalised in eight domains.
These include: (1) respect for the dignity of persons; (2) autonomy to participate in health- related decisions; (3) confidentiality; (4) prompt attention; (5) adequate quality of care; (6) communication; (7) access to social support networks; and (8) choice of health care providers.
COSTA RICAS HEALTH CARE SYSTEM IS GROSSLY NEGLIGENT AND UNRESPONSIVE DUE TO THE WHO’s INTERVENTION:
Herein we outline the failure of the Costa Rican health system under the direction of the WHO and outlines overwhelming cause for invoking the Constitution Article 46 prohibition on private monopolies in the public interest, and for fully reforming the WHO to be responsive to vulnerable stakeholders, or withdrawing from the WHO as a member state.
In this report, we propose how the very concept of “global governance” is antithetical to the constitutional concept of a personally responsible government that is responsive to the needs of those it’s seeks to serve. Public Health is good owed to all individuals, and as such it requires a far more responsive system than the Ministry is providing to us.
The net result of the unresponsive public health system is a one size fits all diagnostics, prevention and treatment program. This lack of consideration of the differences in people is causing systemic loss of equal treatment in health, with most individuals having documented loss of health and social protections.
These same domains of public health responsiveness have been recognized in the context of human rights and the provision of health services to the public.
Human rights provide a vitally important framework for examining these domains. Like principles of ethics, human rights provide or support appropriate standards for human conduct. Yet, unlike some ethical principles, human rights are internationally recognized and globally accepted. Moreover, governments have agreed to be legally bound to upholding principles of human rights.
Human rights are deliberately broad and elastic to allow for limited differences in interpretation based on cultural or religious beliefs. "While the significance of national and regional particularities and various historical, cultural and religious backgrounds must be borne in mind, it is the duty of States, regardless of their political, economic and cultural systems, to promote and protect all human rights and fundamental freedoms.”
Consequently, the terminology and concepts underpinning human rights are particularly appropriate in providing a normative framework for measuring the domains of health systems responsiveness.
We first discuss these domains by referring to provisions in international human rights instruments, including the human right to health. We further analyze the ways that the understanding of these domains may be enhanced through an understanding of their underlying human rights principles.
Below we briefly outline the failure of health responsiveness under WHO’s direction, and why the failure is reinforcing a grave systemic violation of human rights, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
The grave systemic violation of human rights caused by nation states strict adherence to WHO policy is revealing itself to be a national security threat under Siracusa Principles Article 32: “The systematic violation of human rights undermines true national security and may jeopardize international peace and security”.
(1) respect for the dignity of persons;
Respect for the dignity of persons, including the rights to security & freedom from discrimination
Respect for the dignity of persons in the delivery of public health and individual health services is a core component of health system responsiveness because it protects each individual from potential abusive practices, bodily infringements, and mental harms. Respect for dignity is also a consistent theme in human rights. The first article of the UDHR proclaims the important role of dignity: “All human beings are born free and equal in dignity and rights.” (Human Rights and Public Health in the AIDS Pandemic (OUP Oxford 1997) vii). As eloquently articulated by the UN High Commissioner for Human Rights and Executive Director of UNAIDS:
It is not necessary to recount the numerous charters and declarations ... to understand human rights ... All persons are born free and equal in dignity and rights. Everyone ... is entitled to all the rights and freedoms set forth in the international human rights instruments without discrimination, such as the rights to life, liberty, and security of the person, privacy, health, education, work, social security, and to marry and found a family. Yet, violations of human rights are a reality to be found in every corner of the globe (13).
In human rights terms, dignity implies a bundle of rights and freedoms ensuring that all individuals are treated with respect and remain free to pursue their own hopes and dreams. Human rights doctrine also protects human dignity in quite specific ways as the following discussion illustrates.
In human rights law, the doctrine of informed consent is entrenched under the right to security (14) and is pivotal to respecting the dignity of persons. Thus, for example, competent adults are empowered to make inherently personal decisions, such as whether to accept or refuse medical treatment. The doctrine of voluntary consent to medical tests, treatment and research also arises from other norms and agreements. Notably, there are numerous ethical standards for protecting the dignity of human subjects, including the Nuremberg Code, Declaration of Helsinki, and Guidelines of the Council of International Organisations of Medical Sciences (CIOMS), all of which is not considered in the current covid-19 WHO response.
Perhaps the most important way of ensuring human dignity is to fight invidious discrimination. Discrimination on the basis of race, sex, religion, ethnicity, political views, property, birth, disability, or other status is deeply hurtful to the human condition. The International Bill of Rights strongly promotes the right of non-discrimination in numerous covenants and declarations. ICCPR, Article 26 illustrates:
All persons are equal before the law and are entitled without any discrimination to the equal protection of the law. In this respect, the law shall prohibit any discrimination and guarantee to all persons equal and effective protection against discrimination on any ground such as race, color, sex, language, religion, political or other opinion, national or social origin, property, birth or other status.
The right not to be subject to discrimination is especially important in health care and public health. Since health services are so fundamental to human well-being, they must be allocated fairly among all persons and based primarily on need.
The WHO and their alliance of media, social media, pharmaceutical and financial monopolies are currently persecuting and censoring medical experts through the ‘Trusted News Initiative’, with no due process or warning. People are even having their entire social media platforms and payment gateways removed for people who exercise freedom of speech that contradicts WHO’s official positions. A new term called ‘cancel culture’ has arisen from the UN-WHO policies which is completely antithetical to the UN’s alleged purpose of protecting human rights and a free world.
It cannot be overstated that the ‘Trusted News Initiative’ and UN’s ‘program to combat misinformation and rumors’ are not in conformity with law and as applied ubiquitously worldwide, is a clear overreach and violation of the UN charter and international Human Rights norms.
The use of the term “in conformity with the law” in Article 21 of the ICCPR, should not be interpreted to imply any lower standard of legality for limitations on the right of peaceful assembly than other limitations within the ICCPR. It should be the same standard that applies to interpreting the language of “provided by law” within Article 19 of the ICCPR, as elaborated in the Committee’s General Comment No. 34:[1] “For the purposes of paragraph 3, a norm, to be characterized as a “law”, must be formulated with sufficient precision to enable an individual to regulate his or her conduct accordingly and it must be made accessible to the public. A law may not confer unfettered discretion for the restriction of freedom of expression on those charged with its execution. Laws must provide sufficient guidance to those charged with their execution to enable them to ascertain what sorts of expression are properly restricted and what sorts are not.”
The laws regarding ‘health misinformation’ do not describe what exact speech is defined as health misinformation, in order to: a) be able to challenge the validity of the science and law to know if its really true or false misinformation (with a final res judicata judgment) and b) to give due process to the people that WHO is applying global censorship to. As a result, the WHO-UN global censorship programs (‘Trusted News Initiative’ and UN’s ‘program to combat misinformation and roumers’) that indisputably confers unfettered discretion for the restriction of freedom of expression on those charged with its execution is in violation of the legal order and absolutely null. Importantly, the creation and execution of the global UN-WHO ‘Trusted News Initiative’ and UN’s ‘program to combat misinformation and roumers’ should ultimately be determined to systematically deny human rights which is a national security threat in all nations.
[1] HR Committee, General Comment No. 34 on Article 19: freedoms of opinion and expression, CCPR/C/GC/34, 12 September 2011; at para. 25.
Conclusion: The persecution and censorship of scientific debate and even peer reviewed studies being suppressed by the WHO is a systematic denial of the human right to equal treatment by design which is reinforcing a grave systemic violation of human rights, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
(2) autonomy to participate in health- related decisions;
Human rights support the autonomy of individuals to participate fully in health-related decisions. This ties into key human rights principles such as freedom to seek, receive and impart information (ICCPR, Article 19) and the right to free, meaningful and effective participation (Declaration on the Right to Development, 1986, Article 2) in decisions which affect one's development. Consistent with the formulation of ethical principles, moreover, which underlie the relationship of HCWs and health researchers with their patients, freedom of choice is an essential quality in the delivery of health services. As stated above, the right to security of persons requires that for an individual to provide meaningful consent to medical procedures, she must be fully informed of the risks and purposes of the medical intervention. In the absence of complete and objective information, an individual cannot make an autonomous decision about one's medical services. Furthermore, like principles of ethics, human rights recognize the need for the individual to be fully capable of making health-related decisions. Persons must be competent to make these decisions. That is, the person must be able to understand the basic nature and purpose of treatment to make an informed decision. Persons who lack competency (e.g., persons with significant mental or intellectual disabilities) are entitled to the assistance of others (e.g., parents, caregivers) to help make a decision that is in their best interests. These findings derive directly from human rights instruments concerning the rights of children and the mentally disabled. Under the Convention on the Rights of the Child, for example, the child's best interests shall be a primary consideration in all actions taken and his or her views should be heard and taken into consideration. (CRC, Articles 3 & 12). Thus, human rights support an individual’s autonomy with regard to participation in health- related decisions and being fully informed, in the context of a person being capable of making decisions based on available information.
Participation mechanism insufficient - Participatory government under Article 9 & right to participate in health: “[t]he principle of participation and inclusion means that people are entitled to participate in decisions that directly affect them, such as the design, implementation and monitoring of health interventions. Participation should be active, free and meaningful” (WHO, 2011)
Because the WHO is actively refusing to consider the majority of scientists and peer reviewed studies, the WHO’s decisions appear to be based on cherry picked and biased preconceived presumptions. Due to the recently implemented in 2020 ‘Trusted News Initiative’ and global censorship, both sides of the scientific debate are not being heard, denying meaningful participation. Scientific data is not being considered by WHO, with no motivation or analysis, which would normally be debatable facts and part of the scientific process, as well as the health practitioners right and duty to participate and collaborate with Health Ministries and the WHO in a free and open society. By excluding the scientific groups evidence and information of existing ordinary treatments, diagnostics invalidity and safety signals the WHO is in clear violation of IHR Article 12 4. In determining whether an event constitutes a public health emergency of international concern, the Director-General shall consider: (d) scientific principles as well as the available scientific evidence and other relevant information.
The lack of WHO actually reviewing the available scientific evidence and other relevant information that scientists are trying to impart is very problematic. The validity of the WHO’s declaration of a pandemic is reliant upon methods of diagnostics that are not in conformity with the unequivocal rules of science. For instance, WHO first recommended PCR testing for diagnostics at 45 ct, which is a cycle threshold found too high to detect an active infection, and unscientific. The basis of the alleged covid-19 pandemic is the cases confirmed by using the PCR test at 45ct, which is a test that is now withdrawn and outdated because it is discredited in a peer reviewed study found valid by multiple courts, and even by the WHO and Minesterio de Salud themselves, agree the test is “unable to diagnose an active infection”, “cant tell flu from covid” and “stays active for months, even when no longer contagious”.
The fact is that WHO declared the covid-19 emergency based solely on an unscientific test they chose and recommended.
The WHO and Health Ministries worldwide (penetrated by WEF-UN-WHO) are denying peer reviewed science that conclusively proves WHO guidance is unscientific. This denial of contradictory science is an omission tantamount to fraud that is causing a systematic denial of human rights, including the right of health practitioners and citizens to participate in science and public health policy.
Governmental or private sector limits on the communication of health information may infringe on individual freedom to exchange information. UDHR, Article 19 states: “Everyone has the right to freedom of opinion and expression; this right includes freedom to . . . seek, receive, and impart information and ideas through any media and regardless of frontiers.” Freedom of expression may be violated by a government law that prohibits the dissemination of health data to patients or others at risk of adverse health consequences.
This exclusion of experts by the WHO is intentional and omits true science by design, which is reinforcing a grave systemic violation of human rights, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
(3) confidentiality;
Privacy and confidentiality
Respect for persons in the health care context includes the duty to keep a patient’s medical information private and confidential. Article 12 of the UDHR specifically recognizes the right to privacy: “No one shall be subjected to arbitrary interference with his privacy, family, home or correspondence.” The European Court of Human Rights has also recognized the right to privacy in several cases (15). The human right to privacy means that patients should have substantial control over how their intimate health information is shared with others. In the health care setting, privacy and confidentiality refer to the patient’s right to expect that HCWs or others will not improperly access, use, or disclose identifiable health data without the person’s consent. Health data may include not only a patient’s sensitive health status, but also those facts or circumstances that the patient reveals to HCWs as part of seeking medical treatment. Thus, for example, where a patient living with HIV/AIDS reveals that he may have contracted the virus by sharing needles with other injecting drug users, this statement should be held in confidence even though drug use may be illegal. As with the doctrine of informed consent, the right to privacy and confidentiality must be applied sensitively, with respect for different cultural, social, and religious traditions.
Conclusion: The WHO’s attempt to create a global bio-surveillance network to gather medical information which they suggest should be used in exchange for entry to social establishments, is advocating the denial of the human right to medical privacy, denies equal treatment and is discriminatory by design, which is impermissibly reinforcing a grave systemic violation of human rights in many countries, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
(4) prompt attention;
This responsiveness domain refers to having timely service so as to avoid potential anxiety and inconvenience created by any delays in receiving attention or care. It remains a separate issue from receiving prompt medical attention in a life-threatening situation. Most of the human rights literature refers to the need of patients to receive prompt medical attention, especially in cases of emergency where access to medical care is critical. The preservation of life is a fundamental human right (UDHR, Article 3; ICCPR, Article 6). Whenever an individual’s life is jeopardized by her medical status, a human right to life supports the obligation of the state to assure that medical attention is accessible and provided. The European Court of Human Rights (16) and domestic courts such as the Supreme Court of India (17) have affirmed that the right to life encompasses a right to adequate health care in an emergency. Closely linked to the right to life is the right to health, which incorporates access to basic health services as an important pillar. The importance of ensuring access to health service in complying with obligations under the right to health supports the notion of "prompt attention" (18) which is used in the responsiveness domains. In particular, the issue of accessibility has been articulated in General Comment 14 adopted by the UN Committee on Economic, Social and Cultural Rights. Accessibility in this literature has four overlapping dimensions: non-discrimination, physical accessibility, economic accessibility and information accessibility. Two of these dimensions relate to the domain of prompt attention, namely, non-discrimination and physical accessibility. Non-discrimination with regards to health facilities means that goods and services must be accessible to all, especially the most vulnerable or marginalized sections of the population, in law and in fact, without discrimination on any of the prohibited grounds. With regard to physical accessibility, accessibility means that goods and services must be within safe physical reach for all sections of the population, especially vulnerable or marginalized groups, such as ethnic minorities and indigenous populations, women, children, adolescents, older persons, persons with disabilities and persons with HIV/AIDS. Accessibility also implies that medical services and underlying determinants of health, such as safe and potable water and adequate sanitation facilities, are within safe physical reach, including rural areas. Accessibility further includes adequate access to buildings for persons with disabilities. This last issue links with the domain of basic amenities.
The lack of prompt attention by WHO to experts providing contradictory information required for the preservation of human life and to provide the public adequate and truthful information is a systematic denial of the human right to equal treatment by design which is reinforcing a grave systemic violation of human rights, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
(5) adequate quality of care;
Adequate quality of basic amenities
This domain links to the right of everyone to an adequate standard of living for himself and his family, including adequate food, clothing and housing, and to the continuous improvement of living conditions including healthy and edible food (ICESCR, Article 11). In addition, the General Comment on the Right to Health which articulated the normative content of ICESCR, Article 12, underscored that health facilities, goods and services must be of quality which includes, inter alia, safe and potable water, adequate sanitation and access for all to work and thrive financially.
Conclusion: UN and WHO recommended shutting down “non essential” work, which is a systematic denial of the human right to equal treatment, dignity and safety in financial interests required for nutrition and health, which is reinforcing a grave systemic violation of human rights, creating a sequele of global poverty, business shutdowns and bankruptcy and secondary health issues which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
(6) communication;
Health care analysts have traditionally perceived the quality of health care as the combination of technical and inter-personal measures. A HCW may be technically proficient, but may be viewed by individuals as delivering low quality care because of his or her lack of inter-personal skills, most notably, the ability to effectively communicate with patients. In support of the provision of quality health care, then, the right to health equally sustains the need of public health authorities and HCWs to communicate with patients in ways that benefit the individual. A patient that lacks adequate medical information from her health Ministry and provider cannot make autonomous decisions about her health services or options. Failing to effectively communicate infringes the realization of an individual’s enjoyment of human rights, particularly the right to seek, receive and impart information.
HCWs must be prepared to provide health information to patients in language and format that furthers a patient’s understanding. Thus, a communication to a patient through written correspondence in the patient’s secondary language may be ineffective. Such communication does not allow for interactive discussion or the opportunity to confirm the patient’s receipt or comprehension of the information.
In order to achieve a goal of clear communication to patients, clear communication between health workers is therefore necessary. This helps to address the identified gap of "continuity of care", as the transfer of information between health care workers would impact on the patient's experience of continuity.
Governmental or private sector limits on the communication of health information may infringe on individual freedom to exchange information. UDHR, Article 19 states: “Everyone has the right to freedom of opinion and expression; this right includes freedom to . . . seek, receive, and impart information and ideas through any media and regardless of frontiers.” Freedom of expression may be violated by a government law that prohibits the dissemination of health data to patients or others at risk of adverse health consequences.
Denied truthful information - 3.2.3. Access to accurate health information The rights to health and freedom of expression intersect to require States to provide access to accurate health information about the pandemic (CESCR, 2020a). Information must be accessible to all on the basis of non-discrimination.
WHO’s lack of accurate health and diagnostic information about their declared pandemic is a systematic denial of the human right to equal treatment by design which is reinforcing a grave systemic violation of human rights, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
(7) access to social support networks; and
Access to social support networks, family and community support
Access to social support networks (also referred to as family and community support) can be a key condition for the amelioration of negative health traits among individuals. Individuals with illnesses or disabilities often need assistance in accommodating their conditions at work, home, or public places. Familial or other support helps individuals reach their health goals. Human rights, including respect for the dignity of persons, the right to health, the freedom to associate, and the right to familial assistance (ICESCR, Article 10) generally uphold this need for access. Unwarranted limitations on the ability of a person to seek their family, friends, or others within a social network for support concerning the person’s health status may infringe these rights.
Conclusion: Under the guidance of the WHO dying people are denied family and community support, even denied visits with loved ones, dying alone, when the family poses no risk of covid transmission by being young and no risk or by being naturally immune and recovered already, which is a systematic denial of the human right to equal treatment by design which is reinforcing a grave systemic violation of human rights, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
(8) choice of health care providers.
The realization of human rights, including the right to health, neither requires nor precludes any particular form of government or economic system. The human right to political participation (the right to vote and to take part in the conduct of public affairs) ensures that societies can freely choose the type of system which the peoples residing in it find most conducive to the fulfillment of their rights and needs. The result is that health systems vary in terms of priorities and approaches used and values underpinning both of these. Offering individuals a choice of medical providers is a valued feature of health systems in industrialized countries like the United States (where provider choices, at times, are viewed as excessive). A choice among providers is considered to help improve patient access to care, as well as the quality of care. In terms of international human rights law, however, there are no specific provisions indicating whether a health system should or should not offer choice in terms of medical providers. Human rights provisions are deliberately broad and elastic to allow countries to meet the needs and wishes of their populations in terms of devising systems which fulfill the basic human rights of all the population paying particular attention to the most vulnerable and marginalized.
Conclusion: Since declaring covid-19 a pandemic, the WHO has interfered with the Dr. - patient bond by actively recommending blanket treatment protocol and disapproving of ordinary approved essential medicines that are clinically proven to reduce mortality. The uniform treatment protocols recommended by the WHO are denying individualized health care and fails to consider the differences of people, which is required to provide right to equal treatment in health required. By failing to consider the differences in people and controlling the treatment protocol to ensure blanket one size fits all global medical treatments, and suppression of access to ordinary treatments, the WHO is ensuring that individuals are not being treated with individualized care right for them, which is a systematic denial of the human right to equal treatment by design which is reinforcing a grave systemic violation of human rights, which is a vice or defect that negates the very motive, content and purpose for WHO’s existence.
Enhancing the domains of health responsiveness through reification of the Siracusa Principles and human rights
Each of the health responsiveness domains discussed above in this analysis is arguably supported by one or more principles of human rights. We have attempted to show what human rights principles share with responsiveness domains. Beyond mere support, there are at least three ways that human rights principles enhance these domains.
Synergy; Health authorities and human rights advocates have long extolled the connection between protecting human rights and maintaining human health. As discussed above, human rights and health are synergistic. People need to be healthy to fully enjoy their human rights; respecting human rights encourages healthy behaviors, choices, and options for individual and community health services. The domains of health system responsiveness parallel multiple human rights obligations designed to improve the health status of both individuals and populations. As a result of the WHO’s lack of respecting the domains of health system responsiveness, there is a documented worsening individual and community health outcomes. In other words, human rights theory and principles support the need to deliver health services consistent with these domains not only to improve health outcomes, but also to further a respect for human rights that underlie the intrinsic value of the domains themselves, which requires the prohibition of the WHO in countries wishing to respect health and human rights of their populations, rather than blindly obey the edicts of the WHO which may be causing a national security threat by systematic denial of human rights.
This synergy that is currently obstructed by the WHO’s emergency response suggests the need to conceive and build a less global, more nationalized and rights-based approach to the delivery of health care services. Essentially, responsiveness supports a rights-based approach to health systems as related to the interactions between patients and health systems which is an essential element required for health that the WHO is currently unwilling or unable to satisfy, thus negating the WHO’s very reason for existing.
Authority and accountability; In addition to the need to recognize these domains in the delivery of health services, the field of human rights provides an international set of norms that sustains their acceptance. The WHO’s lack of adhering to these domains in the provision of health services is wholly inconsistent with good health practice that promotes individual and community health, because adhering to these domains in the provision of health services is mandated by human rights. Reframing these domains in terms of human rights obligations offers an additional, authoritative justification for public and private sectors to respect these domains. Failures of the UN-WHO to respect these domains may lead to human rights violations that may be reviewed by international tribunals, constitutional and other courts, human rights monitoring bodies, or through public juries, assemblies and public opinion. Violations of human rights carry similar and sometimes additional penalties, as would legal violations. The potential for direct or indirect response assigns a degree of accountability against those who infringe or violate human rights, including the WHO employees acting as de facto public employees while advising governments under emergency powers. When fairly enforced, human rights provide a universal standard that holds governmental and other actors accountable.
With the WHO announcing a ‘new normal' under covid-19 emergency powers complete with overt global technocracy controlled centralized censorship, there is a clear potential for biased information. This bias confirmation is certain because the UN and WHO joined WEF the largest public-private monopoly on earth who is partners with Pfizer and AstraZenica, big tech, media, etc. This global privately funded monopoly with WHO as the head of public relations is the controller of the media, the online information stream of official and “allowed” health information, the UN human rights commission, which means the UN-WHO is essentially acting as wrongdoer and simultaneously controlling the information they deem “truth” and are also the acting judge, all in the same proceedings. This is prohibited under common law to be the judge in your own case. The UN-WHO-WEF can propose what is truth or misinformation if they wish, however, under common law false statements are treated as fraud by inducement, with cases requiring an injured party. This system is time immemorial because it presumes most people do not want truth to be centralized in the government or privately funded WHO-UN-WEF global monopoly, historically dignity of man requires free will to weigh both sides of the argument ourselves after confronted with facts and law so each of us can decide for ourselves what to believe or advocate publically.
Conclusion: Having one UN controlled globalized outlet for human rights monitoring (the Human Rights Commission) is a vice or defect that creates the appearance of bias that frustrates the very purpose of human rights monitoring bodies existing as an impartial arbitrator between two separate parties, this lack of impartial oversight of the UN-WHO-WEF is cause for distrust amongst the WHO ‘users and consumers’ of health goods.
Cohesion; In many ways, the eight domains of health system responsiveness are distinct yet related. Respecting the dignity of individuals, for example, includes respecting their autonomy to participate in health-related decisions. It also requires that an individual’s interests in protecting the privacy and confidentiality of her intimate health data be protected. The WHO’s implementation of QR codes and green pass vaccine passports is not only contrary to the unequivocal rules of science, it is gross overreach encroaching into medical privacy rights and is invidiously discriminatory. Human rights analysis affirms the underlying construct of responsiveness, common to all the domains, and bridges any perceived or actual gaps between domains (e.g. the implications of communication for continuity of care). Thus, as discussed above, the human right to health supports the need to provide prompt medical treatment and keeping information private. Failing to deliver on one of these domains for the sake of the other (outside medical or public health emergencies) may be viewed as infringing on the right to health, notwithstanding justifications offered by health care workers or government authorities. In this way, international human rights law provides cohesion to the domains that require HCWs and the WHO to strive to fulfill these components in the delivery of health services.
Because the privately funded WHO is unresponsive and actively works to undermine to the needs of their users and consumers by refusing the rules of science, and censoring health information, the WHO is acting contrary to the interests of the people and global community they seek to serve.
WHO’s history of pandemic Alarmism & non disclosure requires strict scrutiny.
REMINDER OF WHO’s DUTIES:
Compliance, risk management and ethics
This is a friendly reminder of the WHO’s history of documented structural defects:
Council of Europe condemns “unjustified scare” over swine flu
BMJ 2010; 340 doi: https://doi.org/10.1136/bmj.c3033 (Published 07 June 2010)Cite this as: BMJ 2010;340:c3033 Adrian O’Dowd
The Council of Europe has heavily criticised the World Health Organization, national governments, and EU agencies for their handling of the swine flu pandemic.
The parliamentary assembly of the council—the international organisation that protects human rights and the rule of law in Europe—published a draft of a report that reviewed how the H1N1 pandemic was handled. National governments, WHO, and EU agencies had all been guilty of actions that led to a “waste of large sums of public money, and unjustified scares and fears about the health risks faced by the European public,” says the report. The conclusion came in the parliamentary assembly’s social, health and family affairs committee report published on 4 June. The report was prepared by Paul Flynn, socialist member of the assembly and Labour MP for Newport West and approved by the committee ahead of a plenary debate at the end of this month. It says there was overwhelming evidence that the seriousness of the pandemic was vastly over-rated by WHO, which led to a …
MEPs criticise WHO over H1N1 pandemic advice
BMJ 2011; 342 doi: https://doi.org/10.1136/bmj.d652 (Published 01 February 2011)Cite this as: BMJ 2011;342:d652 Rory Watson
The European parliament has launched a strong attack on the World Health Organization, accusing it of distorting the term “pandemic” during the H1N1 outbreak in 2009-10 and triggering a worldwide false alarm. That, in turn, gave rise to inappropriate and disproportionate public health decisions by European Union countries, members of the parliament claim. The criticism comes in a report drafted by the French Green MEP Michèle Rivasi evaluating management of H1N1 flu in 2009-10 in the European Union. The report was overwhelmingly adopted by the parliament’s public health committee on 25 January, with 58 votes in favour of the report, just two against, and one abstention.
WHO admits to “inconsistencies” in its policy on conflicts of interest
BMJ 2010; 340 doi: https://doi.org/10.1136/bmj.c3167 (Published 15 June 2010)Cite this as: BMJ 2010;340:c3167 Zosia Kmietowicz
The World Health Organization has admitted that its policies governing the publication of conflicts of interests of its expert advisers have “inconsistencies” and that safeguards “surrounding engagements with industry” need to be tightened.
The agency was responding to criticisms of its handling of the swine flu pandemic in an investigation by the BMJ and the Bureau of Investigative Journalism and a report from the Council of Europe published last week.
The joint BMJ and bureau investigation found that key scientists advising WHO on planning for a flu pandemic had done paid work for drug firms that stood to gain from the guidance and that the agency had not declared these conflicts of interests (BMJ 2010;340:c2912, 3 Jun, doi:10.1136/bmj.c2912). In addition, …
WHO processes on dealing with a pandemic need to be overhauled and made more transparent
BMJ 2011; 342 doi: https://doi.org/10.1136/bmj.d3378 (Published 31 May 2011)Cite this as: BMJ 2011;342:d3378
The World Health Organization failed to manage possible conflicts of interests between its expert advisers and industry in handling the H1N1 flu pandemic, an independent review panel has found.
The review, chaired by Harvey Fineberg, president of the US Institute of Medicine, concluded procedures were inadequate, should be overhauled, and made more transparent.
The panel found no evidence of “attempted or actual influence” by commercial interests on advice or decisions taken by the WHO concerning the pandemic. But WHO failed to acknowledge legitimate reasons for some criticism, in particular, inconsistent descriptions of a pandemic that “may have inadvertently contributed to confusion and suspicion.”
An investigation published last year by the BMJ and the Bureau of Investigative Journalism (BMJ 2010;340:c2912, doi:10.1136/bmj.c2912) found that key scientists advising the WHO on planning for an influenza …
WHO has not been transparent since at least 2010, when they overreacted and caused “waste of large sums of public money, and unjustified scares and fears about the health risks faced by the European public,”
WHO admits to “inconsistencies” in its policy on conflicts of interest
BMJ 2010; 340 doi: https://doi.org/10.1136/bmj.c3167 (Published 15 June 2010)Cite this as: BMJ 2010;340:c3167
Zosia Kmietowicz The World Health Organization has admitted that its policies governing the publication of conflicts of interests of its expert advisers have “inconsistencies” and that safeguards “surrounding engagements with industry” need to be tightened.
The agency was responding to criticisms of its handling of the swine flu pandemic in an investigation by the BMJ and the Bureau of Investigative Journalism and a report from the Council of Europe published last week.
The joint BMJ and bureau investigation found that key scientists advising WHO on planning for a flu pandemic had done paid work for drug firms that stood to gain from the guidance and that the agency had not declared these conflicts of interests (BMJ 2010;340:c2912, 3 Jun, doi:10.1136/bmj.c2912). In addition, …
European parliament criticises H1N1 pandemic response
BMJ 2011; 342 doi: https://doi.org/10.1136/bmj.d1639 (Published 14 March 2011)Cite this as: BMJ 2011;342:d1639
The European Union parliament has branded as “disproportionate” some of the public health measures that governments took during the H1N1 pandemic two years ago. MEPs have also called on European Union countries to overhaul their prevention plans to make them more effective, coherent, and flexible.
In a strongly worded resolution the parliament urges the World Health Organization to revise the definition of a pandemic to take account not just of its geographical spread but also of its severity.
The resolution and accompanying report were drafted by the French Green MEP Michèle Rivasi. After they were approved on 8 March in Strasbourg she said, “This report…
World Health Organization refutes allegations
BMJ 2007; 334 doi: https://doi.org/10.1136/bmj.39136.486007.FA (Published 01 March 2007)Cite this as: BMJ 2007;334:440
The World Health Organization categorically rejects the allegations made in a recent story in the BMJ which imply that WHO solicits money from the pharmaceutical sector through independent organisations by circumventing its own rules.1 As …
The Shocking ‘Trust WHO’ Margaret Chan confession that the WHO is influenced by the preferences of the funders!!!
This powerful investigative doc uncovers an alarming picture of corruption and opacity as filmmaker Lilian Franck asks whether the organization can be trusted to keep the public healthy.
Notice: Trust WHO? Is a very important documentary on why the WHO is so dangerous and untrustworthy due to being essentially purchased for sale by private funders who’s “donations to the WHO are intrinsically tied to the preferences of the funders”. This is not our speculation.
It is a fact Margaret Chan the last Head of the WHO confessed that, “donations to the WHO are intrinsically tied to the preferences of the funders”,. Conflicts of Interest are a known defect in the WHO's structural integrity according to the last statement in the documentaries final 5 minutes. There is no room for doubt that oversight of the WHO's funders and their policy making power and ‘key player' seats at the table is needed, due to the confession made by the previous head of WHO Margaret Chan in 2017, translated to Spanish.
Trust WHO? 2018
WHOS DOCUMENTED LACK OF INTEGRITY; FALSE STATEMENTS REGARDING SAFETY MECHANISMS!
WHO is documented to have a lack of truth, probity and integrity in their mission of “providing technical support monitoring the health situation and assessing health trends”, a breach so serious it requires strict scrutiny and oversight that is unavailable within the current WHO framework:
WHO Chief Scientist caught lying about vaccine safety:
https://www.bitchute.com/video/cBy9sKYHJfUo/ “
W.H.O. Works to Ensure Vaccinations are Safe” with Dr Soumya Saminathan, promotional video, released November 28, 2019: “Vaccines are very safe. If someone gets sick after vaccination it usually either a coincidence, an error in administering the vaccine, or very rarely a problem with the vaccine itself. That’s why we have vaccine safety systems. Robust vaccine safety systems allow health workers and experts to react immediately to any problems that may arise. They can examine the problem, rigorously and scientifically look at the data, and then promptly address the problem. W.H.O works closely with countries to make sure that vaccines can do what they do best – prevent disease without risks. New vaccines against malaria, meningitis, and encephalitis in Asia and Africa are now being thoroughly monitored with support from WHO Vaccines are one of the safest tools we have to prevent disease and ensure a healthy future for all children.”
Five days later, Dr. Souyma Swaminathan discussed vaccine safety behind closed doors at the W.H.O. Global Vaccine Safety Summit. Geneva, Switzerland, December 3, 2019 “I think we can not overemphasize the fact that we really don’t have very good safety monitoring systems in many countries, and this adds to the miscommunication and the misapprehensions, because we are not able to give clear cut answers when people ask questions about the deaths that have occurred due to a particular vaccine, and this always gets blown up in the media. One should be able to give a very factual account of what is actually happening and what the cause of deaths are, but in most cases there is some obfuscation at that level, and therefore there is less and less trust in the system. Putting in place the mechanisms, whether they are cohort studies or whether they are sentinel surveillance sites, to be able to monitor what’s going on and report back, and then for corrective action to be taken, because unexpected things could arise after introduction. And one always has to be prepared, as we’ve seen in the history of many drugs, you’ve learned about adverse events only after the drug has been licensed and introduced into the population. So I think that risk is always there, and the population needs to understand that, and feel confident that mechanisms are being put in place to study some of those things.”
In the WHO constitution it explains their monopolistic tendencies:
As of 2012, the WHO has defined its role in public health as follows:
providing leadership on matters critical to health and engaging in partnerships where joint action is needed;
shaping the research agenda and stimulating the generation, translation, and dissemination of valuable knowledge;
setting norms and standards and promoting and monitoring their implementation;
articulating ethical and evidence-based policy options (while censoring experts evidence);
providing technical support (cherrypicked), catalyzing change, and building sustainable institutional capacity; and · monitoring the health situation and assessing health trends.
CRVS (civil registration and vital statistics) to provide monitoring of vital events (birth, death, wedding, divorce).
Mandatory Constitutional notice Article 46:
We are a body established for the purpose of defending our rights that we are entitled to under Article 46 and Article 9 to participate. This includes our right to participate in the design, implementation and final decisions of any health policy which may affect our right to health, environment, safety and financial interests; to receive adequate and truthful information; to freedom of choice and to equal treatment.
ARTICLE 46. Private monopolies and any acts, even if originated by law, which may threaten or restrict freedom of trade, agriculture or industry, are prohibited.
Action by the State aimed at preventing any monopolistic practices or tendencies is in the public interest.
Companies organized as de facto monopolies shall be governed by special legislation.
The establishment of new monopolies on behalf of the State or the Municipal Governments shall require the approval of two- thirds of all the members of the Legislative Assembly.
Consumers and users are entitled to the protection of their health, environment, safety and financial interests; to receive adequate and truthful information; to freedom of choice and to equal treatment. The State shall support any bodies established for the purpose of defending their rights. The law shall regulate those matters.
(As amended by Article 1°, Law No. 7607, May 29, 1996.)
WHO is promising the following:
WHO - Accountability and funding
We are committed to the principle of accountability – a core value for an organization that is entrusted by countries and other donors to use limited resources effectively to protect and improve global health.
Accountability is vital for the success of any organization, especially one that asks the nations of the world to entrust it with their funds, pledging to use them to improve health globally.
It’s even more vital in a world marked both by increasing competition for limited development resources, and by greater scrutiny of results obtained. Countries and other donors rightly want to know what their contributions are achieving.
WHO- our values https://www.who.int/about/who-we-are/our-values
Persons of integrity
We practice the advice we give to the world
We engage with everyone honestly and in good faith
We hold ourselves and others accountable for words and actions
References
Endnotes
1 Murray CJL, Frenk J . A framework for assessing the performance of health systems. Bulletin of the World Health Organization 2000, 717-731
2 Vienna Declaration and Programme of Action, Article 1.
3 Vienna Declaration and Programme of Action, (United Nations General Assembly document A/CONF.137/23) adopted at the World Conference on Human Rights, Vienna, 14-25 June 1993, par. 5.
4 See, e.g., Henry J. Steiner and Philip Alston. International Human Rights In Context: Law, Politics, Morals. Oxford Univ. Press, NY; 1996: 59-117.
5 See, e.g., The Convention on the Elimination of All Forms of Discrimination Against Women (1979).
6 See, e.g., The Convention on the Rights of the Child (1989).
7 See, e.g., International Convention on the Elimination of All Forms of Racial Discrimination (1969).
8 See, e.g., United Nations. HIV/AIDS and Human Rights International Guidelines (September 1996).
9 See, e.g., The United Nations Declaration on the Rights of Persons with Mental Illness (1991).
10 Steven D. Jamar. The International Human Right to Health. Southern University Law Review 22 (Fall 1994): 1-68, citing UN Doc. A/CONF. 32/8.
11 Jonathan Mann, Lawrence O. Gostin, Sofia Gruskin, et al. Health and Human Rights, J. Health and Human Rights 1994;1:6-22.
12 United Nations Economic and Social Council (ECOSOC) (1985). The Siracusa Principles on the limitations and derogation provisions in the international covenant on civil and political rights. UN Doc. E/CN.4/1985/4, Annex.
13 Peter Piot & Jose Ayala-Lasso. Foreword to Lawrence O Gostin & Zita Lazzarini Human Rights and Public Health in the AIDS Pandemic (OUP Oxford 1997) vii.
14 Lawrence O. Gostin & Zita Lazzarini. Human Rights and Public Health in the AIDS Pandemic (OUP Oxford 1997) 14-15.
15 See, e.g., Dudgeon v United Kingdom (No 2) (1982) Series A No 45 (1982) 4 EHRR149.
16 Paul and Audrey Edwards v United Kingdom, Application no 46477/99 (14 March 2002).
17 Paschim Banga Khet Mazdoor Samity v. State of West Bengal, Supreme Court of India, AIR 1996 Supreme Court 2426.
18 Committee on Economic, Social, and Cultural Rights (CESCR), General Comment No. 14. The right to the highest attainable standard of health (May 2000); Geneva.
(1) Transforming our World: The 2030 Agenda for Sustainable Development.
UN General Assembly. 2015. 21 October. UN Doc. A/RES/70/1.
(2) General comment No. 20: Non-discrimination in economic, social and cultural rights
Committee on Economic, Social and Cultural Rights. 2009.
(3) Guiding principles for business and human rights, Implementing the United Nations “Protect, Respect and Remedy” Framework
Office of the high Commissioner for Human Rights, Geneva, 2011.
(4) CESCR General Comment No. 14: The Right to the Highest Attainable Standard of Health (Art. 12)
CESCR (Committee on Economic, Social, and Cultural Rights). 2000. ). 11 August. Doc. E/C.12/2000/4.
Costa Rica’s unresponsive health system under the WHO - with all downloads
The Above Document was sent to the WHO on May 2, 2022, is part of our formal charges against W.H.O. Staff because all presumptions must be refuted or they stand in law.
The full ‘IOJ Stakeholder Engagement Packet’ can be downloaded here.
Most information herein is taken from the old WHO document “Human rights and health” issued on 29 December 2017 (we UPDATED and added to the concepts for accuracy and to remind the WHO of their duties to human rights obligations):
Ways You Can Help Stand Up To The Madness Of The W.H.O. Meeting This Week To Amend The IHR Global Health Policy By Removing Respect For Dignity, Human Rights And Fundamental Freedoms:
Sign and share the following actions so your voice will be counted in IOJ’s real legal actions! Together they are forced to listen to us when we act as a group!
#1 Click To Sign The Legal Demand To Stop The IHR Amendments
Sign HERE to officially protest the IHR Amendments being negotiated THIS week that literally seeks to cross out and eliminate “respect for dignity, human rights and fundamental freedoms”.
Sign NOW! Its more important than most people realize.
#2 Click To Sign The Legal Demand To Hold W.H.O. Staff Accountable For Crimes Against Humanity
Sign HERE to support IOJ’s CRIMINAL Charges for crimes against humanity and breach of ethics against key W.H.O. Staff Director General and Chief Scientist (and her successor Jeremy Farrar). Support our charges already filed (and not yet answered by WHO) for PCR fraudulent statistics, false declaration of pandemic that violates international law, as well as the unilateral and void definition of vaccine that allows gene therapy with unreasonable risks to be mislabelled globally as a vaccine, in excess of W.H.O. authority, knowing it cannot actually PREVENT DISEASE, required for all vaccines, to the detriment and harm of the international community and public interest.
DO YOU AGREE ITS TIME TO SUE THE W.H.O. FOR INTERNATIONAL WRONGDOING AND BREACH OF ETHICS & RESEARCH STANDARDS DUTIES?
#3 Click To Donate And Support The Cause
IOJ is a small organization fighting global corruption which exists due to the Awesome support of donors. Because we are truly independent with no government or corporate funding our ongoing legal work against W.H.O., FDA and Wrongdoer States needs YOUR HELP to be able to continue. Please support the real people behind the scenes to do this work if you are called to do so and able. We really need your help financially right now (and throughout this year) to impede the oppressors in a real legally binding way.
We are proud to do this mission of freeing humanity, but its a TON of work and we need all conscious freedom fighters to know IOJ is small and we are NOT funded. We need your support to continue and we believe we can win with each one of your support.
Would you consider a donation of $100-$1000. or more to ensure IOJ’s legal fund is at a level to be able to do our job of crushing the dreams of tyrants in 2023?
Everyone wants to be able to change the world, including ourselves, but how will it be paid for?
TELL EVERYONE YOU CAN TO HELP SUPPORT IOJ WHICH IS JUST A MOM N POP SHOP!
We love you tribe and supporters! We have your back & humanities! Thanks for having ours.
We can still win this in 2023 if we take persistent action together.
Thank You!
https://t.me/InterestOfJustice ~Telegram
Check out IOJ’s Public Participation Videos in front of WHO, FDA, HHS OGA:































There is an insidious global ruling class plot to enslave all life on earth behind all the madness and suffering inflicted on We the People.
How to fight back against this TOTAL SLAVERY! ABOLISH THE WHO, THE WEF, etc.
RESIST! DO NOT COMPLY! DITCH THE DAMNED 'SMART' PHONES AND THE DAMNED QR CODES AND GO BACK TO LANDLINES OR FLIP PHONES AND USE CASH AS MUCH AS POSSIBLE! INSIST ON CASH! CBDC IS TOTAL SLAVERY!
Other than getting rid of nuclear weapons which I support 100% the rest of the anti-nuclear peace movement and CLIMATE CRISIS propaganda is parroting UN utter GARBAGE, a complete surrender to the ENSLAVEMENT AGENDA by the diabolical despots of Davos - ruling class criminals who lust for total power and control and all of whom should be tried and jailed for life and their malign organizations dismantled: the UN, the WEF, the IMF, the WHO, the BIS, NATO, Blackrock, Vanguard, The Rockefellers, the Rothschilds, The Bilderbergers, the CFR et al.
There is an evil predator globalist technocratic elite agenda of eugenics/depopulation/genocide using bioweapon poison jabs, war, geoengineering, EMF radiation, starvation and economic collapse - THE GREAT RESET/AGENDA 2030/4TH INDUSTRIAL REVOLUTION to get rid of billions of 'useless eaters' and to use nano tech to turn the survivors into ROBOTIZED COMPLIANT SLAVES! WAKE UP AND RESIST! DO NOT COMPLY! These are psychopath megalomaniacs who want to play god by turning all life into digitized metaverse mechanistic synthetic biology to be manipulated by their AI algorithms. A more demonic sickening idea is nearly impossible to imagine!
APPALLED AND HORRIFIED AT INSANE TYRANNICAL PROTOCOLS THAT HAVE NOTHING TO DO WITH HEALTH AND EVERYTHING TO DO WITH TOTALITARIAN CONTROL! REVERSE THIS NOW!
MAKE THE WORLD AND AMERICA 2019 (comparatively speaking), AND FREE AGAIN!
NO, I AM NOT AFRAID OF THE MORONIC SCARIANT SHMARIANT MONKEYSHINES! WAKE UP ALREADY!
TOTALLY CONDEMN BIDEN AND ALL OTHER POLS WHO HAVE NO POWER TO LAWLESSLY ACT LIKE AN EMPEROR OR DICTATOR AND DECREE JAB CROW 'SHOW ME YOUR PAPERS' FASCIST SEGREGATION/DISCRIMINATION/APARTHEID VIOLATIONS OF THE CONSTITUTION, THE NUREMBERG CODES AND EVERY CIVIL RIGHT IMAGINABLE.
NO GREEN NEW DEALS OR BUILD BACK BETTER FROM THE CRIMINAL TECHNOCRAT TYRANTS KLAUS SCHWAB AND HIS CRONIES FROM THE WORLD ECONOMIC FORUM.
STOP THE TERRIBLE TYRANNY OF THE TECHNOCRATS GLOBAL AGENDA OF TOTAL SURVEILLANCE AND CONTROL USING THE VIRUS AS EXCUSE AND PROPAGANDA TOOL!
NO MUZZLING STIFLING MASK MANDATES! NO FORCED VACCINES! END TORTUROUS DEVASTATING LOCK DOWNS NOW! I WANT MY LIFE BACK.
https://wrenchinthegears.com
https://www.stopworldcontrol.com/
https://www.thelastamericanvagabond.com
https://pandemicfacts.info
https://wearehumanwearefree.org/7-days-campaign/
https://sonsoflibertymedia.com/covid-19-roadmap-12-step-plan-to-create-a-totalitarian-new-world-order-were-on-number-8-headed-towards-number-9/
https://questioningcovid.com
https://www.corbettreport.com/interview-1581-james-corbett-breaks-down-the-great-reset/
http://www.stopcp.com/GlobalResetPSYOP/GlobalResetPSYOPMindMap.html
https://everydayconcerned.net/2020/09/04/breaking-major-investigative-report-by-association-of-french-reserve-army-officers-finds-covid-19-pandemic-to-have-a-hidden-agenda-for-global-totalitarianism-nanotech-chipping-of-all-5g-irradia/
Pam Popper: https://makeamericansfreeagain.com
Del Bigtree: https://www.brighteon.com/channels/highwire
https://www.technocracy.news
Naomi Wolf: https://dailyclout.io
www.nojabforme.info
https://www.globalresearch.ca/we-must-awaken-from-corona-coma-reject-great-reset-robotic-technocracy-assert-common-humanity/5745213
The fact they do not respond at any charges, they ignore everything and everyone who is not in their line, they push all the unlawful no common sense rules, at a point will force the states, the governments to publicly recognize that they are not what they should be or pretend to be anymore and that they are in the service of the bankers and corporations interests, this is what we are witnessing these days, they can not and they do not guaranty the people's safety, justice and rights. There is no such thing as the "future of democracy", it is democracy or it isn't. Democracy without the rule of law is no democracy, no matter how many word games they are playing.
God bless you! 🙏